July 14, 2017
Written by Bianca Salaverry (class of 2016-2017)
My July OREX day was the most eventful one I’ve had so far. After an interesting morning lecture given by (I think) the chief ortho resident, I got to observe four surgeries.
Surgery 1: This was an irrigation and debridement (I & D) for an infection from a previous surgery. It was a fairly fast procedure, lasting only about an hour and a half. The patient came in because he had undergone surgery on his ankle not long ago and the main incision was infected. The surgeons reopened a two-inch portion of the old incision and basically just flushed it with a ton of saline. The new incision wasn’t very deep, but the doctors did make a small cut into the fascia to make sure there wasn’t any pus, which would’ve indicated a more serious infection. Luckily they didn’t find anything, and the surgery went off exactly as planned.
Surgery 2: This was one of those surgeries where I had to look up some names/acronyms in order to figure out exactly what was going on. I’m always excited by those cases because it means something new I’ve never seen before. The board called it a “Cystoscopy TURBT, and possible biliary ureteral stent placement.” A cystoscopy just refers to the insertion of a camera and light up through the urethra and into the bladder. TURBT stands for transurethral resection of a bladder tumor.
I had a great time observing this surgery because the attending performed the entire thing on her own with no residents around, so she was happy to answer my questions and talked me through a lot of the procedure. The patient came in because he had seen blood in his urine. Imaging showed that he had several large, likely cancerous tumors in his bladder. A major complicating factor here was that the man was morbidly obese. I’ve seen patients this large in the ED, but never in the OR, and once the patient was under, it became very difficult to adjust his position, which ended up being problematic. Even the initial step of inserting the camera into the urethra wasn’t working because the weight of his stomach was compressing his bladder and preventing the camera from entering and moving around easily. They called in a transport team and tried several techniques to adjust the patient. First they moved his whole body down towards the surgeon, which allowed her to insert the camera. She was still having trouble moving the probe around in his bladder though, so then they tried stretching tape from the underside of his belly up towards his shoulders to hoist it up and away from the bladder. All the adjustments added a lot of time to the procedure, which the surgeon wasn’t too happy about.
Once she had access, the doctor started to point out some of the anatomy to me. The normal bladder mucosa was smooth and pink with small blood vessels. In contrast, the tumors were clear/white and had tiny nodules with little pink dots in the center. The shape was similar to the papillary carcinomas shown here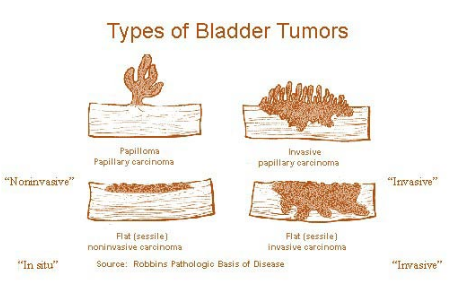 and the picture below is pretty close to what the tumors actually looked like on the camera, though in my case, the bright red vessels were absent.
and the picture below is pretty close to what the tumors actually looked like on the camera, though in my case, the bright red vessels were absent.

In order to remove each tumor, the doctor used a tool to scrape and cut them off the walls of the bladder and break them into smaller pieces. The tool also had suction attached to remove the pieces once they were small enough. In theory, this was supposed to be a fairly simple surgery, but because of the man’s size, it was hard to maneuver the tools in his bladder, and the doctor kept having to pull everything out of the urethra, so what should have taken only a couple of hours stretched on much longer. I didn’t stay until the end because the doctor kept urging me every half hour to go find something more interesting to observe.
Surgery 3: This procedure wasn’t the most eventful, but the injury was probably the strangest one I’ve seen in my whole time at Highland. The ortho surgeons had operated on this patient for a tib/fib fracture a while before (I’m not sure exactly how long, maybe a few weeks?). His wound was totally closed and the man had two ring shaped external fixators placed, one just below his knee and the other closer to his ankle. Apparently the fracture was so bad that the surgeons had to remove an entire segment of his tibia roughly four inches long. I didn’t get a chance to ask too many questions during this surgery, so I still don’t totally understand why the bone fragment was removed, but the aim of this follow-up procedure was to make some adjustments to the external fixator in order to take some strain off of the skin around the injury. I asked Dr. Krosin what the end goal was for the patient and he said that at that point, they were just doing everything they could to prevent having to amputate the man’s leg below the knee.
Surgery 4: My last case of the day was very sad. Everyone in the room was familiar with the circumstances, and some people seemed pretty upset about it. The patient was a young guy who had gotten into a car accident while intoxicated. His son unfortunately died in the accident and the man himself was in the ICU for a while afterwards and didn’t even know his son had died until several days later. He was also severely injured. He had broken both legs in multiple places and had undergone several surgeries already to repair a broken tibia and hip on his right side. This surgery was an open reduction and internal fixation (ORIF) for a femur fracture. I’ve seen several ORIFs during my OREX shifts, and the most remarkable thing about this one is that there were a lot of little pieces of bone that had to be fixated, so the surgeon had to very carefully position each tiny fragment and put the end of the bone back together with the smallest K-wires they had.
There were some tough things to see during my July OREX shift, but days like this one do a lot to remind me how important it is to have compassion for patients in difficult situations, and to remain objective and give everyone the best care possible regardless of the circumstances around their medical issues.
Posted on October 15, 2017, in Uncategorized and tagged cystoscopy TURBT, external fixators, K-wires, ORIF femur fracture, tib/fib fracture, transurethral resection of a bladder tumor. Bookmark the permalink. Leave a comment.
Leave a comment
Comments 0